Compare Weight Loss Surgery Operations
In modern times there is an extensive range of weight loss procedures available.
They essentially differ according to the following properties:
- Safety
- Effectiveness
- Reliability
- Eating experience
- Ease of eating a range of foods
- Amount of data and research available
- Level of maintenance required

Each operation has a different profile mix of the above. Your choice of procedure is based on a range of factors but essentially comes down to your viewpoint on risks and invasiveness of the surgery and the reliability of the eventual outcome. Generally speaking the more complex procedure will likely give the more reliable and substantial weight loss.
Adjustable gastric banding is a relatively safe procedure which does not involve cutting the stomach or rearranging normal anatomy. It is however less reliable than the more complex operations and is a high maintenance procedure involving frequent clinic attendance.
Gastric bypass and SIPS are more complex interventions with a higher possibility of a surgical complication or nutritional compromise. Both are excellent for diabetes and the bypass specifically has decades of experience and study available indicating substantial, reliable weight loss for most.
The sleeve gastrectomy is a relatively newer operation which has a more moderate risk profile and is low maintenance. Weight loss is fairly reliable but long term outcomes are still under a question mark.
Endoscopic procedures are performed through the mouth with a fibre-optic scope and do not involve surgical cuts. They include the Intra-gastric balloon and Endobarrier implantation. These procedures are temporary in the sense that they must be reversed and generally won’t give the same effectiveness of weight loss as the more conventional operations.
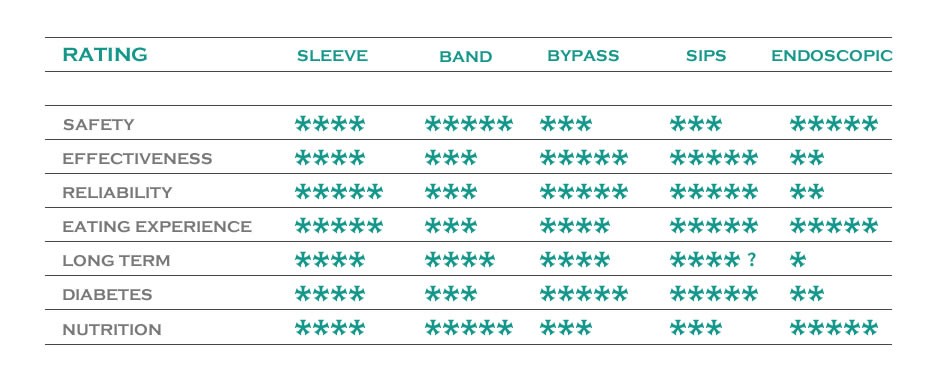
Summary table comparing the main procedures.
More stars means better in that category.
*SIPS means Stomach Intestinal Pylorus Preserving Surgery – a new procedure
Case Studies
Some typical case scenarios are discussed below which may have some similarities to your own circumstances:

22 years old, 110kg, no diabetes
Sleeve surgery is commonly performed in this scenario although there are some issues to consider:
- Although sleeve gastrectomy is an effective operation, it involves removing around three quarters of the stomach and is entirely irreversible. So most of a perfectly good organ is gone for the next 50-60 years of life
- It is possible another treatment (e.g. a tablet) for obesity may appear in say, 20 years or so, but you cannot put back the stomach that has been removed.
- Very occasionally patients have difficult problems such obstruction of the gastric tube leading to ongoing vomiting or perhaps intractable reflux. The only solution may be conversion to gastric bypass leaving very little intact stomach for the rest of the patient’s life.
All operations have their pros and cons in this age group. If the patient is willing to accept a higher operating risk for a more reliable result, gastric bypass is another option for young patients. Although the risks are higher than for banding, no organ is permanently removed and good long term data are available. If a young patient does incur a complication their body will cope better than older patients.

60 y/o, 130kg, on medication for diabetes
- For older patients, gastric bypass can be quite risky as it has the highest complication rate out of the three standard operations discussed although the results are generally good
- Gastric banding is much safer but the average weight loss for older patients is probably only 15-20kg.
- Sleeve gastrectomy is a good option for older patients as the issues regarding lack of long term study data and irreversibility are less important than for younger patients. It gives more reliable outcomes than the band and is effective against diabetes and well as allowing excellent food tolerance which contributes to quality of life
- Endobarrier implantation may be considered in this situation. This device is placed without surgical cuts in a 20 min day procedure using a telescope through the mouth so is relatively safe. It produces moderate weight loss in most with good improvements in diabetes management. It must be removed after 12 months currently however but may be re-implanted if successful.

35 year old, 120kg, dependent on injections for diabetes and treated for high blood pressure
- This young patient is staring down the barrel of substantial health problems by the time they are in their 50s and early death. Weight loss is crucial to get things back under control
- The gastric bypass is probably the most effective procedure for this patient in terms of weight loss and diabetic control. The slightly higher risks of this operation compared to sleeve gastrectomy may be justified by the need for long term reliability and diabetic treatment

35 year old, 95kg, BMI 33, no medical problems
- The medical risks of having a BMI of 33 are not as substantial as patients with BMIs above 40 for example. Therefore it is hard to justify the risks of a stapled procedure in this patient
- This patient may consider weight loss medications such as duromine and should try a range of commercial programmes for weight loss prior to considering surgical intervention
- If the patient is motivated and well educated a gastric band may be an option if all else has failed
- Endobarrier® implantation might be considered but the device must be removed after one year and its effects against diabetes are not useful here
Some of the Weight Loss Surgery Procedures Mr Clough offers.