Gastric Sleeve Discussion
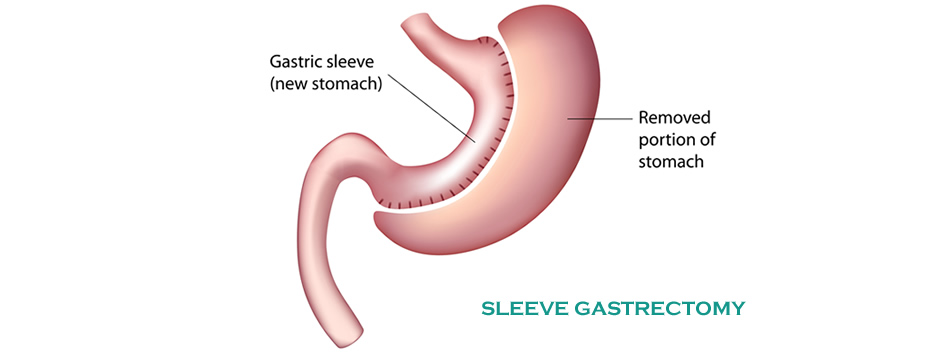
Gastric sleeve has been performed laparoscopically in bariatric centres as a stand alone procedure for around 8-10 years. The reason for the first sleeve gastrectomies was to take some initial weight off very large individuals so that the second stage of their operation (biliopancreatic diversion with duodenal switch) could be safely performed.
Sleeve surgeons found, however, that the sleeve surgery itself was associated with significant weight loss and therefore the second stage was often not required. More recently surgeons have switched to making the residual stomach smaller than the original sleeves were.
Other names for sleeve gastrectomy include vertical sleeve, gastric sleeve and tube gastrectomy.
Most patients qualifying for Gastric Sleeve surgery will have BMI greater than 40, or 35 if there is diabetes, blood pressure, sleep apnoea or other obesity related condition present. Severe reflux symptoms or the presence of Barrett's oesophagus (precancerous cells in the lower oesophagus) will generally mean sleeve is not recommended.
A Banded Sleeve gastrectomy is also available.
Overnight Sleeve Package
Our evidence based MCBS Overnight Sleeve Package ($16,990) caters for uninsured patients who are willing to undertake most of their recovery in their own home in the company of a responsible carer. For more information please follow this link.
For a DETAILED discussion about key medical literature underpinning the current status of Sleeve Gastrectomy surgery click here
Standard Five port Sleeve Gastrectomy (Anthony Clough, sleeve surgeon Melbourne)
The current popularity of the sleeve is because of the following:
- The reliability of weight loss is excellent
- The rate of weight loss is often faster than with gastric banding
- There is usually substantial hunger suppression after sleeve surgery
- The risks of surgery are less than for gastric bypass and it can be done with a keyhole approach almost all the time
- There is usually little in the way of food intolerance and vomiting is not common
- You are less likely to have ongoing issues which may require reoperations (e.g. slipped band) than for gastric banding or bypass.
The down-sides of sleeve gastrectomy are…
- It is irreversible and involves permanent removal of around three quarters of an otherwise perfectly normal organ
- Although results are usually good at the two to three year mark like most weight loss operations, some degree of weight regain will often occur thereafter.
- If weight regain does occur, conversion to gastric bypass may be an option, however this is a big undertaking and leaves even less viable stomach remaining
- Very occasionally (<5%) patients have ongoing issues with vomiting and food intolerance after sleeve gastrectomy. This may be due to a narrowing or twist in the tube and may be difficult to fix
- Leaks can occur from the staple line in up to 2% of cases. These can be difficult to treat and require many weeks or months in hospital
- Some people get acid reflux after sleeve gastrectomy or worsening of pre-existing reflux. It is normally well controllable with medication.
NB: for Sleeve Gastrectomy patients who may have had relatively poor results or regained weight, the loop duodenal switch revision or SIPS surgery may be an option to get things back on track
All you need to know about Sleeve Gastrectomy – short version (left), comprehensive (right)