For my Main Gastric Sleeve Page Click Here
5 Myths of Gastric Sleeve
Myth 1 - If you eat too much you will stretch your stomach
For most sleeve patients, it’s normal for portion sizes to increase somewhat after the first year or so. If significant weight regain occurs the volume of the sleeve could have increased, however often the sleeve looks completely normal when examined by endoscopy. The correlation between a larger sleeve and weight regain is not clear cut. It is unlikely that patient eating behavior makes much difference to long term sleeve volume changes.
Myth 2 -I will lose all my excess weight after the sleeve operation
Many people assume that the sleeve will allow them to achieve “normal” weight again. Although there are people who achieve 100% loss of excess weight after sleeve the majority will eventually stabilize around 60-65% of excess lost. Generally speaking lower BMI patients (e.g. 35-40) are like to achieve higher percentage of excess lost compared to high BMI patients (>50 for example).
Myth 3 - Stitching the staple line will prevent leaks
A specialized device is used to cut and seal the sleeved stomach utilizing three rows of tiny titanium staples. Some surgeons like to oversew the whole stomach staple line from top to bottom. Many patients ask whether the stomach can be stitched to prevent leaks. Unfortunately stitching over the staple line has been shown not to prevent leaks and in some cases could even narrow the sleeve.
Myth 4 - You Can’t Have a Sleeve Operation if You Suffer Reflux
There is no doubt that sleeve gastrectomy can lead to reflux symptoms in some patients or worsen it in others. However the opposite can also be true; sometimes reflux actually improves after sleeve, particularly when the patient loses weight. It is quite unpredictable. Patients with severe reflux or Barrett’s oesophagus (pre-cancerous cells related to chronic reflux) should probably avoid sleeve however and consider bypass instead. Those with mild or moderate reflux will probably be fine.
Myth 5 - A smaller calibration tube is better
The size of the sleeve is broadly determined by the diameter of the calibration tube used to staple around. Commonly used calibration tube sizes range from 32Fr (smaller) to 40Fr (larger)*. There is controversy over weight loss outcomes and complication rates with different tube sizes. Many surgeons feel that smaller calibration tubes lead to more complications (obstructions, leaks) and the larger tubes may given similar weight loss results.
*Fr = French (3x the diameter in millimetres)
MEDICAL LITERATURE
Below is an in depth discussion of some of the most important MEDICAL LITERATURE relating to Sleeve Gastrectomy.
Be warned it is heavy in NUMBERS, GRAPHS and STATISTICS and not for the faint hearted!
For a simpler outline of Sleeve Surgery please navigate to my main Sleeve Gastrectomy Page.
EXECUTIVE SUMMARY
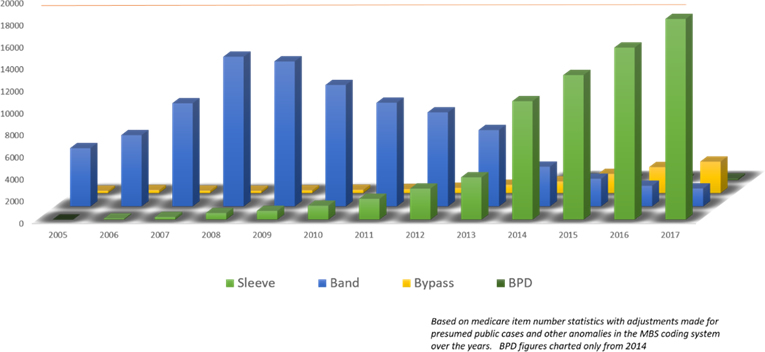
- Sleeve gastrectomy case numbers rose rapidly in Australia from 2013 onwards, effectively replacing Lap Band numbers which fell dramatically over the same period
- Long term loss of excess weight after sleeve averages about 60-65% (excess weight = the proportion of weight you carry above healthy weight range)
- Up to a quarter of patients may require second surgeries to achieve this weight loss or treat reflux over a ten year period
- Studies show less heart attacks and other cardiac events in those undergoing bariatric surgery
- For type II diabetics, sleeve gastrectomy is powerful in improving control or providing remission from diabetes. Much more powerful than drug treatment alone.
- More than one study indicates there may be significant long term survival benefits with bariatric surgery
- New research indicates that the risk of Barrett’s oesophagus may be higher in sleeve patients as compared to the general population. Barrett’s oesophagus refers to cell changes in the lower oesophagus related to chronic reflux which may be precancerous. Sleeve patients therefore may be advised to undertake routine gastroscope surveillance around five years after the sleeve is done.
Sleeve Case Numbers - Australia
Sleeve has now been performed in high volumes around the world for almost 10 years.
This chart shows estimated gastric sleeve cases performed in Australia with the green columns representing sleeve operations and the blue Lap Band. Worldwide trends have roughly mirrored this rise in terms of the recent dominance of the sleeve operation.
Outcomes
Long Term Weight Loss
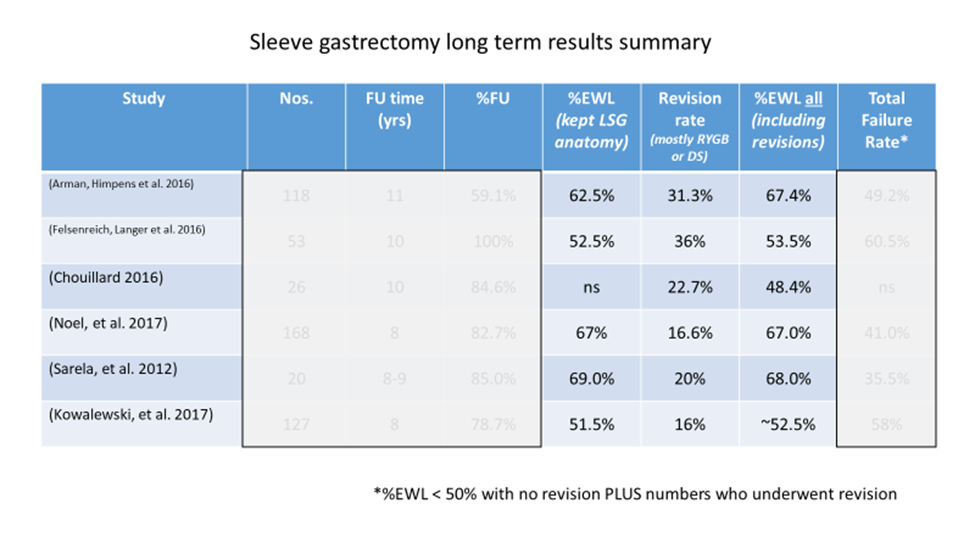
For the statistically minded, a chart below summarises six of the longer term outcomes from sleeve surgery published in the medical literature.
The key figures are highlighted in the chart below:
%EWL = Percentage of Excess Weight Lost. Excess weight is the weight you carry over and above your healthiest weight. LSG = Laparoscopic Sleeve Gastrectomy (i.e. the Sleeve operation)
Key Points:
Weight loss
Patients are achieving on average around 60% of Excess Weight Loss (EWL)* with follow-up times between 8 and 10 years post sleeve.
Revision operation
Around a quarter of patients have required a form of revision surgery over this time period. Mostly this is conversion of the sleeve to gastric bypass surgery either due to reflux symptoms or inadequate weight loss.
Long Term Survival Benefits
Do you live longer because of weight loss surgery? More research is coming out in support of this. Data from two respected studies are presented below.
The study from JAMA (Journal of American Medical Association) shows mortality rates over time comparing around 7500 morbidly obese patients having no surgery versus around 2500 patients who did undergo bariatric surgery. The chance of dying (from any cause) over ten years was around 25% for the obese group who did not undertake surgery (!). Death risk was about HALF of this for the surgical group.
These are REAL figures published in one of the most respected medical journals in the world.
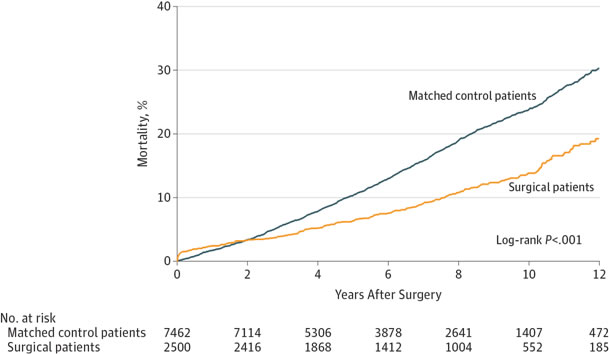
From JAMA. 2012 Jan 4;307(1):56-65. doi: 10.1001/jama.2011.1914.
SOS Study
The SOS study (Swedish Obese Subjects) shows a similar trend although not quite so dramatic. This study compared over 2000 obese patients who underwent surgery against 2000 who didn’t.
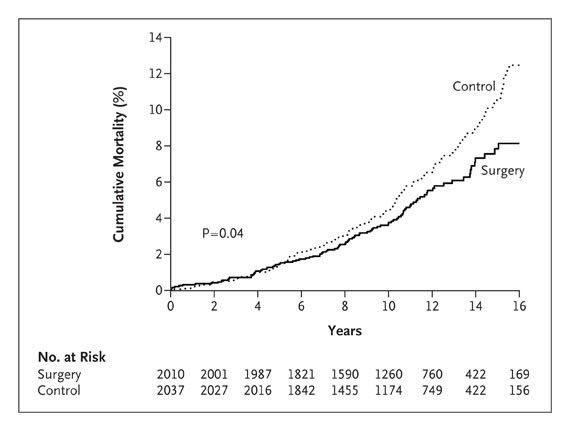
Again, survival over time clearly favours those undertaking bariatric surgery.
Note these survival studies are not specific to sleeve gastrectomy, rather a range of bariatric surgical procedures.
Diabetes Resolution
Type II diabetes responds well to sleeve gastrectomy surgery.
This study from New England Journal of Medicine is probably the best to demonstrate its benefits.
Reference: N Engl J Med 2017;376:641-51.
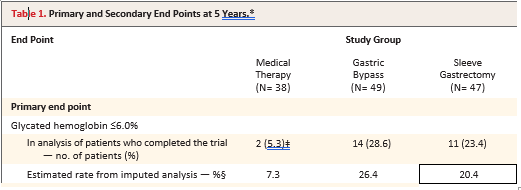
This well designed “randomized” study compares obese patients with poorly controlled type II diabetes undergoing best drug treatment to those undergoing sleeve or bypass surgery. Follow-up is now up to five years after the operation.
This graph excerpt shows the percentage achieving normalisation of diabetes – in this case defined as Hba1c (glycated haemoglobin levels) less than 6.0%. The bottom line of the chart shows about 20% (boxed number bottom right) of sleeve patients achieving this compared to only 7.3% taking best drug therapy.
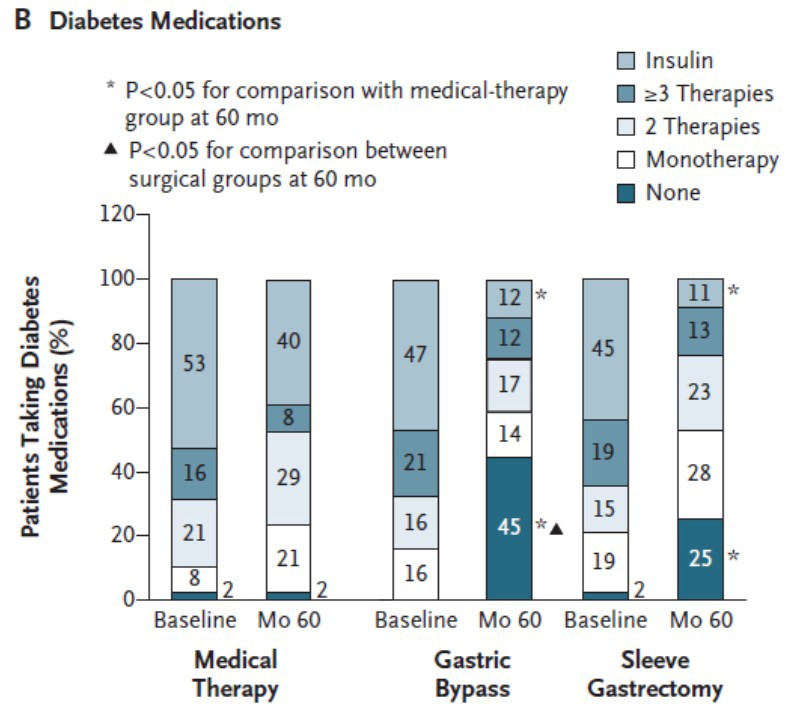
In terms of diabetic medication reduction after surgery, this complicated chart (below) demonstrates how medication reduction can be achieved with the sleeve. The “25” in the bottom right corner in the dark blue segment indicates that 25% of poorly controlled diabetics ended up on no medications at all after sleeve surgery compared to only 2% without having surgery.
Cardiovascular Events
Weight loss surgery can reduce your chance of having a heart attack.
This study from Journal of American Medical Association compares obese individuals undergoing weight loss surgery against those that didn’t. The solid line on the charts indicates the number of cardiovascular events (total – right, fatal – left) experienced over many years compared to those who didn’t undergo the surgery.
The difference is significant and favours those who underwent surgery.
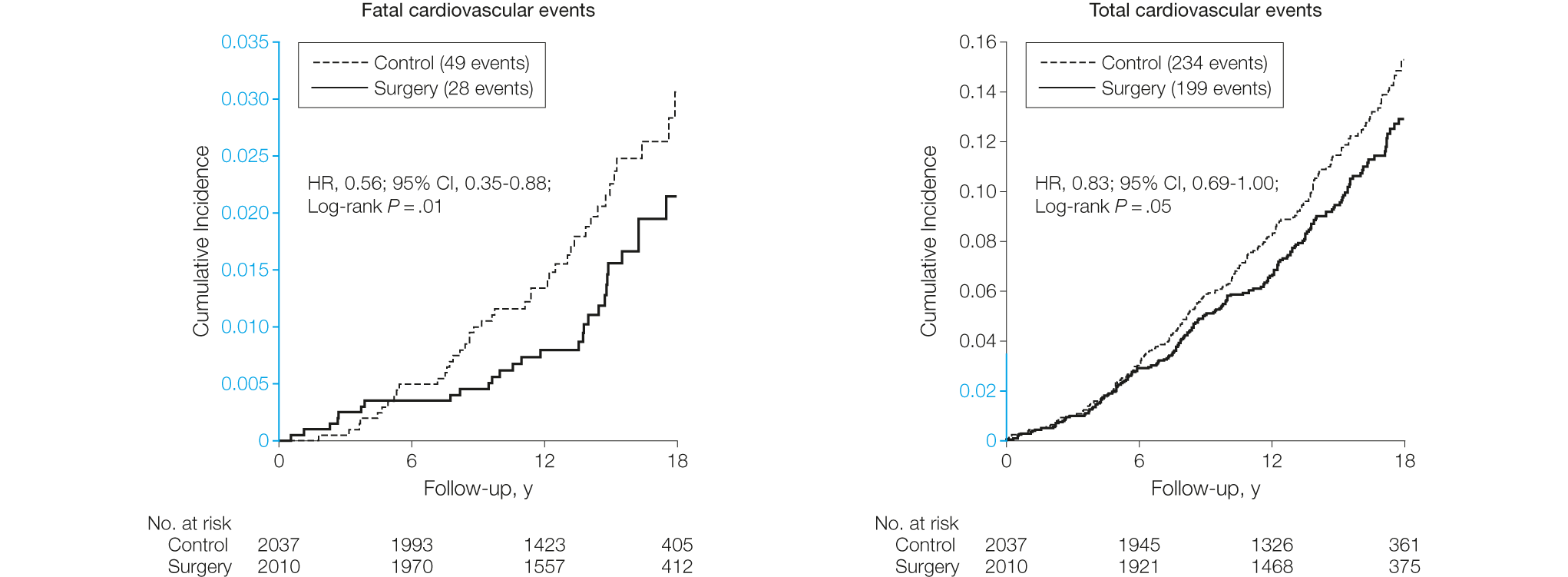
Reference:
Bariatric Surgery and Long-term Cardiovascular Events JAMA, January 4, 2012—Vol 307, No. 1
ADVERSE EFFECTS
Reflux and Barrett’s Oesophagus
Sleeve gastrectomy can cause reflux symptoms in some patients, for example, heartburn or acid volume in the mouth. In others who already have reflux symptoms it can lead to resolution of the symptoms. This is quite unpredictable.
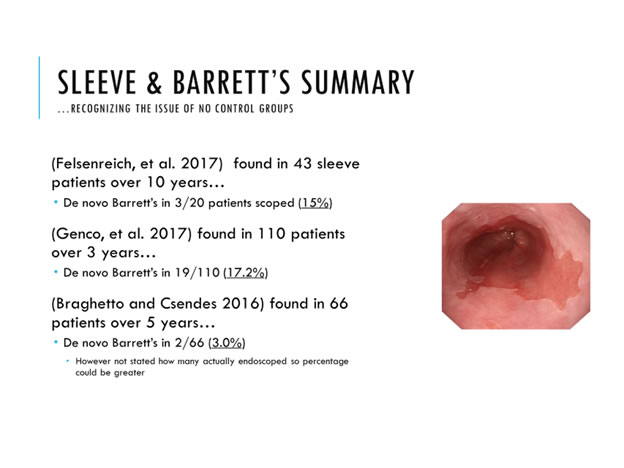
However new information is emerging about increased rates of “Barrett’s oesophagus” after sleeve surgery. Barrett’s oesophagus refers to changed cells in the tissues of the oesophagus to protect itself from acid reflux due to the sleeve. These cells are technically pre-cancerous although cancer actually arising is still quite rare.
Overall your cancer risk (particularly in women) is likely to be much reduced with significant weight loss as obesity is a significant risk factor for a number of cancers.
My policy currently is to recommend gastroscopy at five year intervals after sleeve surgery whilst this issue is under investigation. Gastroscopy can assess for the presence of Barrett’s tissue and biopsies can be taken to ensure there is no risk of cancer progressing.
For the statistically minded, some of the studies are summarised below:
My Sleeve Gastrectomy Comprehensive Video Shown Below